#WHWWeek is April 1 - 7
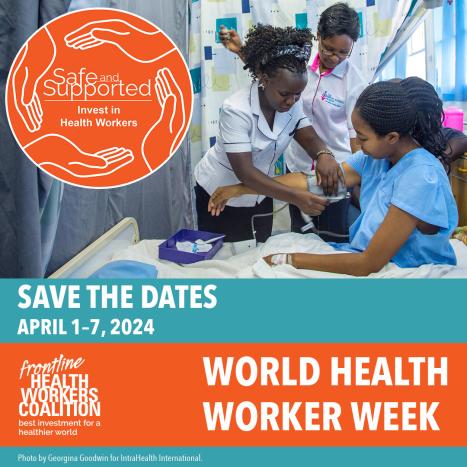
Mark your calendars! World Health Worker Week is April 1 - 7 and the theme is Safe and Supported: Invest in Health Workers.
This World Health Worker Week will bring together advocates, health workers, leaders, and communities around the world to call for greater funding and faster implementation of policies to protect and support health workers–especially women.
The largest global campaign on health workers, World Health Worker Week reached more than 15 million people in 2023. Help us reach even more policymakers and influencers this year.